We might all have something to learn from people who get better, says Mark Eltringham, a former heroin user who now works at a Middlesbrough GP practice that specialises in addiction
‘I’m going to get off this shit, you know. Had enough of it. Know what I’m going to do? I’m going to be a drug worker.”
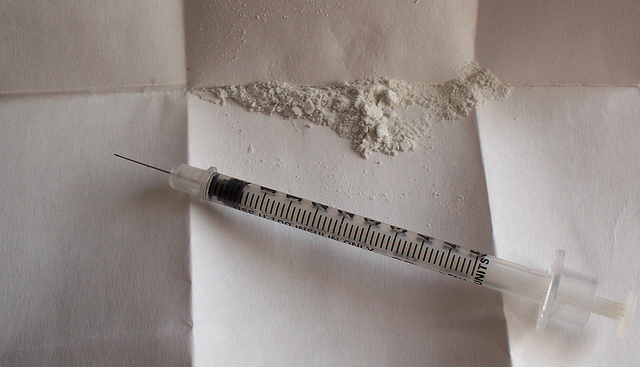
I’ve lost count of number of times somebody I was taking drugs with would come out with a statement like that. My response would vary from “Why would you want to spend all day listening to people like you banging on?” to “Have you finished with that crack pipe?” or “You got my cit?” (Cit or citric acid is used to prepare heroin for injection) to raised eyebrows. Mostly the eyebrows.
I always thought it was a cliché that people went from service users to workers in treatment services, or why some service-users think it’s so important, (“You don’t understaaaaaand”). But somehow I became one.
Of the people I used to hang around with in the 15 or so years that I was a heroin user on Teesside, I’m the only one who made that transition. I think part of the reason is that I’m interested in how it works (or doesn’t) but also how it fits into society. The lifestyle choices of a morbidly obese type 2 diabetic look like poor ones to me and are possibly more harmful (and less fun) than taking loads of class As. But there are interesting parallels in what works as a treatment for people with mild depression, obesity, heart disease, high blood pressure etc and what works as treatment for substance misusers: namely appropriate medication and a mix of some peer support and some learning to think about your thinking. Something to keep you busy might help too.
Along with, sometimes, specialist counselling help. That’s what we’re trying to do at Fulcrum, a GP practice in Middlesbrough that specialises in addictions. I’m not a drug worker and I don’t want to be. I’m interested in why people get better (why me?) and what services can do to improve that. One of the things they can do is use their time and resources better which is why I love the job I now do. I’m lead of a small team that works front-of-house. It’s early days but the idea is that when someone arrives, they don’t just get a prescription and ten minutes with a key-worker. I’m not dismissing that, but there should be stuff going on in the waiting room that they can interact with while they’re waiting. If they need blood, vaccinations, access to another part of the service, we sort that. These are sometimes chaotic people who have complex health needs.
But also the thinking about your thinking, the keeping you busy, the peer support, referrals to specialist counselling. The age profile of heroin-users is shifting. It’s people in their 30s, 40s and 50s who use our services and they’re dying. One of the things we’ve been working on to stop that is take home Naloxone kits. Naloxone temporarily reverses the effects of an overdose and gives time for paramedics to attend. We offer training to service users and their families and prescriptions for the kits.
There’s a subtle but important thing going on here too. Service users are likely to be using the kits on others. Suddenly they’re potentially the person who saves a life. To somebody who doesn’t think much of themselves, that’s hugely important. Suddenly, they can be a hero.
We can all get better: I believe that. But we might all have something to learn from people who get better.
Mark Eltringham is a health improvement worker at Fulcrum Medical Practice. You can follow him on Twitter.
Tell us your views and experiences in the comments section below – by clicking on the little speech bubble.
(Views expressed on our website and in our magazines and emails are not necessarily endorsed by The Northern Correspondent.)